Subscribe to Pittwire Today
Get the most interesting and important stories from the University of Pittsburgh.Long after someone with COVID-19 tests negative for the virus, physical symptoms can persist. So can behavioral ones, it turns out.
Long-haul symptoms — those lasting longer than three months after a negative test — can range widely from person to person: persistent aches and pains, coughing, shortness of breath, brain fog, loss of taste and smell, sleep difficulty, the list goes on. As many as one-third of these patients also continue to struggle with mental health issues, some for the first time in their lives. Since the beginning of the pandemic, studies have shown a high rate of new onset anxiety and depression in people who tested positive for COVID-19.
“A lot of people didn’t have very bad COVID, but continue to have a wide range of significant symptoms,” says Alison Morris, division chief of pulmonary, allergy and critical care medicine at the University of Pittsburgh.
“These symptoms are very stressful to people. They are suffering. We know this. However, with no tested therapies for these conditions, some patients may believe the symptoms are not real and are just ‘in their heads.’”
Morris directs UPMC’s Post-COVID Recovery Clinic, where an app is being used in clinical trials to help patients dealing with long-haul COVID through behavioral health interventions for more integrated care.
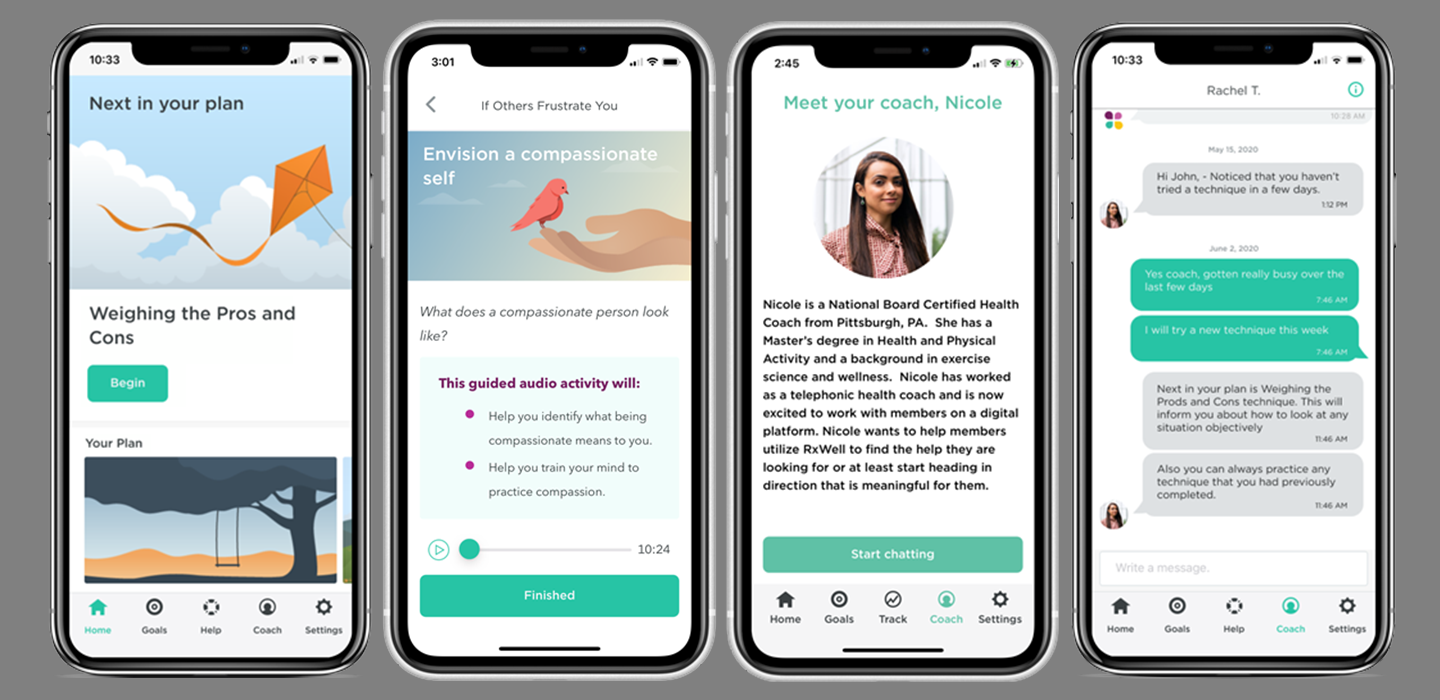
Developed by UPMC Health Plan’s Behavioral Unit for Digitally Delivered Interventions, the app, called RxWell, is a cognitive behavioral therapy (CBT) tool that helps patients deal with the impact of stressors in daily life. The app uses empirically tested CBT and mindfulness techniques for stress, anxiety and depression to help manage symptoms and track progress over time. Patients can work directly with an integrated digital health coach or on their own.
Since 2015, Eva Szigethy, a Pitt professor of psychiatry, medicine and pediatrics, who is the behavioral health director of UPMC’s chief medical office, had been involved in testing RxWell within the UPMC health care system and beyond. Before the pandemic, the app’s usage was associated with reduction in anxiety and depression over three months, Szigethy says, “with an effect size consistent with any psychotherapy trial looking at short-term improvement for mild to moderate mental health issues.”
Since summer 2020, the Post-COVID Recovery Clinic has been enrolling people in Institutional Review Board-approved trials when they are initially diagnosed with coronavirus to gather data about persistent symptoms in conjunction with mood and behavioral health. COVID long-haulers showing initial anxiety or depression are offered RxWell as part of their treatment plan. Those patients with inadequate response to the app are then offered a structured psychiatric consultation to evaluate whether a psychotropic medication is the next-best step.
While there are no results yet, Morris says, anecdotal reports indicate that RxWell is helping people.
“Digital behavioral tools are a dime a dozen these days,” Szigethy says. “Many startups are creating these tools out in the world; they are mainly self-guided, without the regulatory standards or ability to link to many other care coordination efforts to increase their reach and effectiveness.” RxWell, however, is embedded into the electronic medical records system, so it’s easy for clinicians to order it for UPMC Health Plan members and to track a patient’s progress.
“While scientists are still trying to figure out the underlying biology of long-haul COVID, how it manifests and can be treated differently in individuals, RxWell helps get patients to a higher level of behavioral intervention by taking full advantage of the medical system where we can provide stepped care,” Szigethy says.
— Micaela Corn