| front |1 |2 |3 |4 |5 |6 |7 |8 |9 |10 |11 |12 |13 |14 |15 |16 |17 |18 |19 |20 |21 |22 |23 |24 |25 |26 |review |
 |
All chronic complications are related to metabolic alterations activated by prolonged elevated blood glucose levels. When blood glucose levels are kept under control, research has shown significant decrease in the risk of long term complications of diabetes.
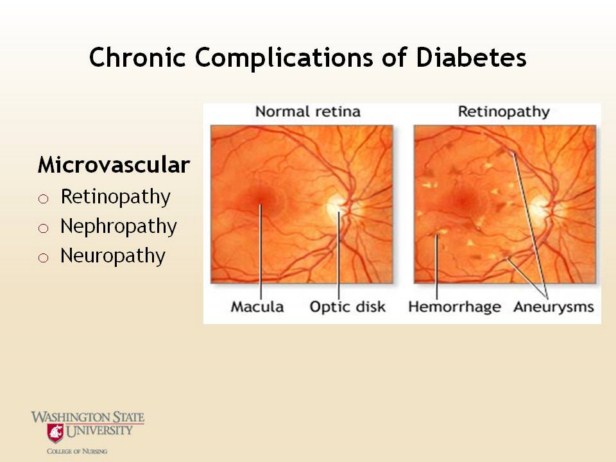
Retinopathy:
1.Diabetic
retinopathy is described by the changes that occur in the retina,
including microanueurysms, hard exudates, soft exudates, hemorrhages and
peripheral retinopathy.
2.Duration
of the disease is linked to Type 1, also with Type 2, but not studied as
much.
3.Influenced
by genetics: HLA DR3 and DR4 predispose for the development of this
complication.
4.African
Americans and Hispanics are more likely to develop than Caucasians.
5.Modified
risk factors include: hyperglycemia, hypertension, dyslipidemia,
abnormal mirocirulation and smoking
6.Retinopathy
damages blood vessels in the retina, the light-sensitive tissue at the
back of the eye that translates light into electrical impulses that the
brain interprets as vision.
●
Nephropathy:
1.The
microvascular complications of diabetes: retinopathy and nephropathy are
thought to result from abnormal thickening of the basement membrane in
muscle capillaries. Capillary basement thickening has been shown to
increase with the length of time after diagnosis and with persistent
hyperglycemia.
2.Nephropathy
affects 30% of Type 1 and 4-20% of individuals with Type 2. Diabetic
nephropathy accounts for 36% of cases of end stage renal disease
(ESRD). Ethnic origins is a risk factor in the development of diabetic
nephropathy, with African American and Native Americans experiencing an
increased of ESRD as compared with Caucasians.
3.Characteristic
lesion of diabetic nephropathy is glomerulosclerosis or thickening and
hardening of the basement membrane of capillaries in the glomeruli.
4.Filtration,
an essential component of kidney function occurs in the glomerulus.The
first stage of diabetic nephropathy is an increase in the glomerular
glow rate, or the rate of blood flow through the glomerulus. This
increased rate leads to hyperfiltration in the glomerulus or a rise in
the rate at which the blood is filtered. As hyperfiltration progresses,
the glormeruli become damaged, which leads to leaking. Protein is seen
in the urine, at first as small amounts (microalbumin) and then grossly
(happens when you dip the urine). As nephropathy advances, the
glomerular filtration rate drops and renal failure happens.
5.There
is evidence that the use of ACE I may reduce the incidence or slow the
progression of nephropathy. They reduce the pressure going into the
glomeruli as well as reduce resistance within the glomeruli.
6.Modifiable
risk factors: Hypertension, dyslipidemia, eating habits, smoking and
frequent UTI
●
What is diabetic kidney disease? Diabetic kidney disease (diabetic nephropathy) is a complication that occurs in some people with diabetes. In this condition the filters of the kidneys, the glomeruli, become damaged. Because of this the kidneys 'leak' abnormal amounts of protein from the blood into the urine. The main protein in the blood that leaks out from the damaged kidneys is called albumin. In normal healthy kidneys only a tiny amount of albumin is found in the urine. A raised level of albumin in the urine is the typical first sign that the kidneys have become damaged by diabetes. Diabetic kidney disease is divided into two main categories, depending on how much albumin is lost through the kidneys: Microalbuminuria. This is when the amount of albumin that leaks into the urine is between 30 and 300 mg per day. Microalbuminuria is sometimes called incipient nephropathy. Proteinuria This is when the amount of albumin that leaks into the urine is more than 300 mg per day. Proteinuria is sometimes called macroalbuminuria or overt nephropathy.
Neuropathy: Neuropathy is defined as either peripheral neuropathy or autonomic neuropathy. The most common cause of neuropathy in clinical practice is diabetes.
Peripheral neuropathy: Develops in more than half of long term diabetics. Diabetes causes several types of neuropathy, which include chronic symmetrical polyneuropathy, proximal neuropathy (diabetic amyotrophy) and mononeuropathies. The pathogenesis of diabetic neuropathies is poorly understood. Many of them have an ischemic basis. A prominent finding in diabetic neuropathy is thickening of arterioles due to increased deposition of basement membrane material, similar to changes that occur in brain arterioles and glomerular capillaries.
Autonomic neuropathy: Affects the nerves in your body that control your body systems. Affects your digestive system, urinary tract, sex organs, heart and blood vessels, sweat glands, and eyes.
Reference: Pathophysiology, 3rd edition: Copstead and Banasik
Image used with permission of AllRefer Health http://health.allrefer.com http://medicalimages.allrefer.com/large/diabetic-retinopathy.jpg |