| front |1 |2 |3 |4 |5 |6 |7 |8 |9 |10 |11 |12 |13 |14 |15 |16 |17 |18 |19 |20 |21 |22 |23 |24 |25 |26 |27 |28 |29 |30 |31 |32 |33 |34 |35 |36 |37 |38 |39 |40 |41 |42 |43 |44 |45 |46 |47 |48 |49 |50 |51 |52 |53 |54 |55 |56 |57 |58 |review |
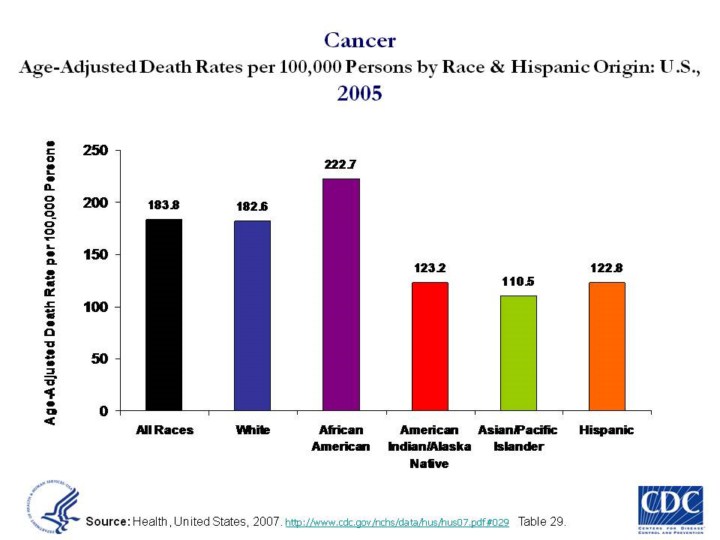 |
Updated 6/2/08 by SB. Age-Adjusted Death Rates per 100,000 Persons by Race and Hispanic Origin for All Causes: U.S., 2002 Compelling evidence that race and ethnicity correlate with persistent, and often increasing, health disparities among U.S. populations demands national attention. Indeed, despite notable progress in the overall health of the Nation, there are continuing disparities in the burden of illness and death experienced by African Americans, Hispanics/Latinos, American Indians and Alaska Natives (AI/ANs), and Native Hawaiian and Other Pacific Islanders (NHOPIs), compared to the U.S. population as a whole. Current information about the biologic and genetic characteristics of minority populations does not explain the health disparities experienced by these groups compared with the white, non-Hispanic population in the United States. These disparities are believed to be the result of the complex interaction among genetic variations, environmental factors, and specific health behaviors. (1)
The death rate for African Americans is 2.3 times as high as for AAPIs, and 1.3 times as high as for white Americans. African Americans have comparatively high death rates for many of the leading causes of death, such as cardiovascular disease (CVD), Diabetes, and AIDS. (JW)
Multiple factors contribute to racial/ethnic health disparities, including socioeconomic factors (e.g., education, employment, and income), lifestyle behaviors (e.g., physical activity and alcohol intake), social environment (e.g., educational and economic opportunities, racial/ethnic discrimination, and neighborhood and work conditions), and access to preventive health-care services (e.g., cancer screening and vaccination). Recent immigrants also can be at increased risk for chronic disease and injury, particularly those who lack fluency in English and familiarity with the U.S. health-care system or who have different cultural attitudes about the use of traditional versus conventional medicine. Approximately 6% of persons who identified themselves as Black or African American in the 2000 census were foreign-born. (8)
For blacks in the United States, health disparities can mean earlier deaths, decreased quality of life, loss of economic opportunities, and perceptions of injustice. For society, these disparities translate into less than optimal productivity, higher health-care costs, and social inequity. By 2050, an estimated 61 million black persons will reside in the United States, amounting to approximately 15% of the total U.S. population. (8)
Slide source (9) |