| front |1 |2 |3 |4 |5 |6 |7 |8 |9 |10 |11 |12 |13 |14 |15 |16 |17 |18 |19 |20 |21 |22 |23 |24 |25 |26 |27 |28 |29 |30 |31 |32 |33 |review |
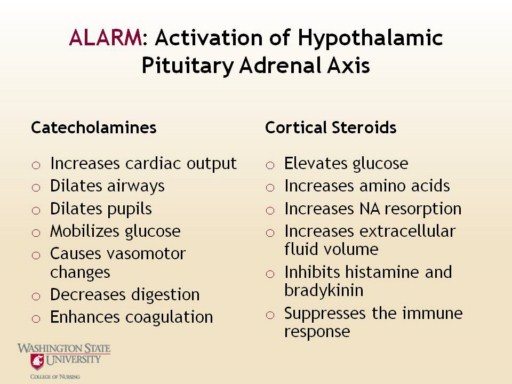 |
The fight-or flight response is initiated. Cells in the hypothalamus produce corticotropin-releasing hormone (CRF). CRF stimulates receptors on pituitary cells to secrete adrenocorticotropic hormone (ACTH). ACTH stimulates the adrenal glands. The adrenal glands secrete cortical hormones and catecholamines. Stress can cause physiological changes that, when sustained, will strain the body’s homeostatic mechanisms, leading to pathogenic conditions. Corticotropin Releasing Factor (CRF) is one of the master triggers of the stress response. Activation of the HPA Axis causes an elevation in catecholamines and cortisol levels. Excessive cortisol has been shown to damage the hippocampus, which is another mechanism that provides negative feedback to the HPA axis. Animal studies have shown that chronic stress results in suppression of neuorgenesis in the hippocampus. People with depression, a very stressful condition, have been shown by MRI to have decreased hippocampal volume. This is important because the hippocampus is involved in short term memory, learning, and contextual memory—helping bind memories together and understand the context. So damage to the hippocampus may impair the ability of a person to understand the stressor. Chronic stress has also been shown to decrease blood flow to the prefrontal cortex. The prefrontal cortex is important to help regulate inhibition. So the person under chronic stress may have a problem understanding the context of the problem, plus a problem controlling their inhibition. This can result in an inappropriate stress response (Southwick, 2007).
|